Don't Panic
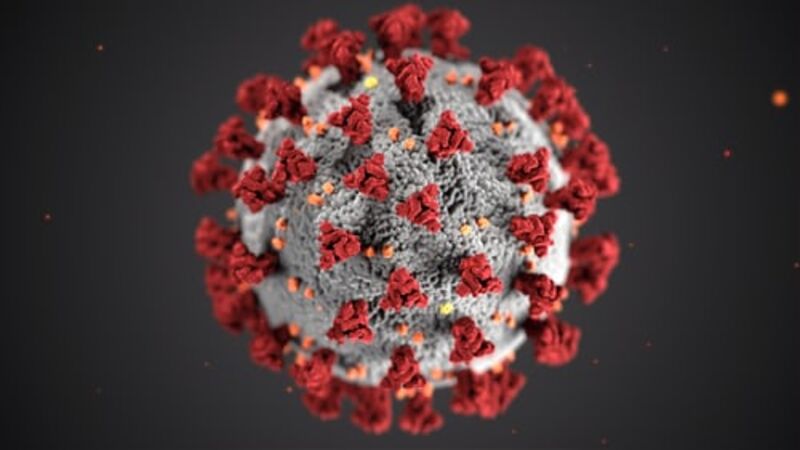
With the increasing numbers of people worldwide infected with the novel coronavirus disease (COVID-19), there is a heightened awareness and hypersensitivity within communities worldwide. On Wednesday, March 11, 2020, the World Health Organization (WHO) named COVID-19 a Global Pandemic. The Center for Disease Control and Prevention (CDC) has a section on their website focused on Coronavirus Disease 2019 (COVID-19).
We should take a step back, breathe and examine the current pandemic. Novel - as it appears in its original name - means new. As with anything that is new, there is a degree of mystery associated with it. As with any mysterious phenomenon, there is a possibility for panic from the public.
So, as the saying goes, "To be forewarned, is to be forearmed!" Let's examine the background of pandemics as opposed to epidemics. In their paper on epidemiology, the CDC gives the following definitions:
- Endemic is the presence of a disease or infectious agent in a population within a geographic area;
- Hyperendemic refers to persistent, high levels of disease occurrence;
- Epidemic is the number of cases of a disease above what is normally expected in that population in that area;
- Outbreak is similar to epidemic but is often used for a more limited geographic area; and
- Pandemic refers to an epidemic that has spread over several countries or continents, usually affecting a large number of people.
Worst Pandemics in History
While the current pandemic may be a cause for concern, one should look back at other outbreaks over the years, with a focus on the 10 worst pandemics in history and then we could make reasonable comparisons:
1. HIV/AIDS Pandemic (At Peak)
Year(s): 2005-2012
Cause: HIV/AIDS
Deaths: 36 million
Result: Ongoing
2. Flu Pandemic (H3N2)
Year(s): 1968
Cause: Influenza
Deaths: 1 million
Result: Contained
3. Asian Flu (H2N2)
Year(s): 1956-1958
Cause: Influenza
Deaths: 2 million
Result: Contained
4. Flu Pandemic (H1N1 - Spanish Flu)
Year(s): 1918
Cause: Influenza
Deaths: 20-50 million
Result: Contained
5. Sixth Cholera Pandemic
Year(s): 1910-1911
Cause: Cholera
Deaths: 800,000+
Result: Contained
6. Flu Pandemic
Year(s): 1889-1890
Cause: Influenza
Deaths: 1 million
Result: Contained
7. Third Cholera Pandemic
Year(s): 1852-1860
Cause: Cholera
Deaths: 1 million
Result: Contained
8. Black Death
Year(s): 1346-1353
Cause: Bubonic Plague
Deaths: 75-200 million
Result: Contained
9. Plague of Justinian
Year(s): 541-542
Cause: Bubonic Plague
Deaths: 25 million
Result: Contained
10. Antonine Plague
Year(s): 165
Cause: Unknown
Deaths: 5 million
Result: Contained
Follow CDC Guidance
Not to nullify the possible impact of COVID-19, the sensible thing to do would be to follow the CDC’s interim guidance on Steps to Prevent Illness:
- Clean your hands often;
- Avoid close contact;
- Stay home if you’re sick;
- Cover coughs and sneezes;
- Wear a facemask if you are sick; and
- Clean and disinfect.
The CDC defines close contact as:
- Being within approximately 6 feet (2 meters) of a COVID-19 case for a prolonged period of time; close contact can occur while caring for, living with, visiting, or sharing a health care waiting area or room with a COVID-19 case; or
- Having direct contact with infectious secretions of a COVID-19 case (e.g., being coughed on).
People with Disabilities and COVID-19
Now, what about people with disabilities and COVID-19? On Sunday March 8, 2020, Forbes published an informative article: 5 Things To Know About Coronavirus And People With Disabilities. This article was also shared on Rocky Mountain ADA Center’s Facebook page on Monday, March 9, 2020. The main takeaway from this article is that having a disability probably doesn’t, by itself, put someone at higher risk from COVID-19. For example, someone who is Deaf or someone who is in a wheelchair is not more likely to be infected than anyone else. However, as the CDC states, those with specific disabilities or chronic conditions may make them more susceptible to COVID-19.
As with any other outbreak, COVID-19 could impact the daily lives of people with disabilities, especially if they depend on others for day-to-day tasks. Examples of Personal Assistance Services (PAS) as outlined by the Office of Disability Employment Policy, might include getting up and ready for work, bathing, dressing, cooking, cleaning, or running errands. Examples of PAS in the workplace vary, but may involve providing travel assistance for an employee with a mobility impairment; helping an employee with a cognitive disability in decision-making; reading printed materials to an employee who is visually impaired; or ensuring a sign language interpreter is present during meetings for an employee who is Deaf.
Who is Susceptible?
The CDC post People at Risk for Serious Illness from COVID-19 focuses on mitigating the effect of COVID-19 on vulnerable members of our population. Such members are older adults and people with serious medical conditions like heart disease, diabetes, and lung disease. These populations would need to take additional precautions to reduce their risk of exposure and sickness.
What Precautions Can We Take?
Most important of all is to have adequate supplies of extra medication, and to have enough household items and groceries on hand in the event one has to self-quarantine at home for a period of time. Other everyday precautions to take would be to avoid close contact with infected people, wash hands often, avoid touching your face, nose, eyes, etc., clean and disinfect frequently touched surfaces, avoid crowds, and avoid all non-essential travel including plane trips.
What does the ADA say about COVID-19?
As COVID-19 is a fairly new phenomenon, and its long-term impact is yet to be felt, we should look at the definition of disability under the ADA. Generally, a flu in and of itself would not be considered a disability for purposes of the ADA. That could change if there are long-term affects to the virus that affects a person’s ability to perform a major life activity.
How does the ADA define disability? Under the ADA, a person has a qualified disability if he or she:
- Has a physical or mental impairment (illness, injury or other condition) that substantially limits one or more major life activities;
- Has a record of such an impairment; or
- Is regarded as having such an impairment.
Each employee’s case needs to be looked at on an individual basis. Generally, it should not be too hard to determine if someone has a disability. However, as an employer, if you need to verify the need for a reasonable accommodation due to a disability that is not obvious, you are allowed to request medical documents related to the request for accommodation. Such medical records would need to remain confidential.
The ADA covers and protects people living with some conditions such as HIV/AIDS, Diabetes, Asthma, Cancer, Cerebral Palsy, Epilepsy, Heart Disease, Multiple Sclerosis, Muscular Dystrophy, Tuberculosis, and others that are usually permanent in nature. On the other hand, it is not yet known if the effects of COVID-19 are permanent. At the time of writing, it is unknown if people who are sick with COVID-19 would be protected under the ADA.
In closure, remember to follow the CDC’s interim guidance on Steps to Prevent Illness:
- Clean your hands often;
- Avoid close contact;
- Stay home if you’re sick;
- Cover coughs and sneezes;
- Wear a facemask if you are sick; and
- Clean and disinfect.